Validating the Invisible: Comprehensive Care for hEDS, Hypermobility, and MCAS
For patients with Hypermobile Ehlers-Danlos Syndrome (hEDS) or Hypermobility Spectrum Disorders (HSD), the road to diagnosis is often long and lonely. A recent global survey of over 3,900 patients found that those with hEDS waited an average of 22 years for a correct diagnosis, while those with HSD waited approximately 17.5 years. Studies from Germany and Australia confirm similar delays, with patients often being told their symptoms are "just anxiety" or that they are simply "deconditioned."
As a rheumatologist, I regularly meet patients who have spent years—sometimes decades—searching for answers to a puzzling array of symptoms. My goal is to help you understand these conditions and recognize when to seek specialized care.
What Are hEDS and HSD?
Think of connective tissue as your body's scaffolding—it's everywhere, providing structure and support to joints, organs, blood vessels, and skin. In hEDS and HSD, genetic variations affect how this tissue behaves, making it more elastic and less stable than it should be.
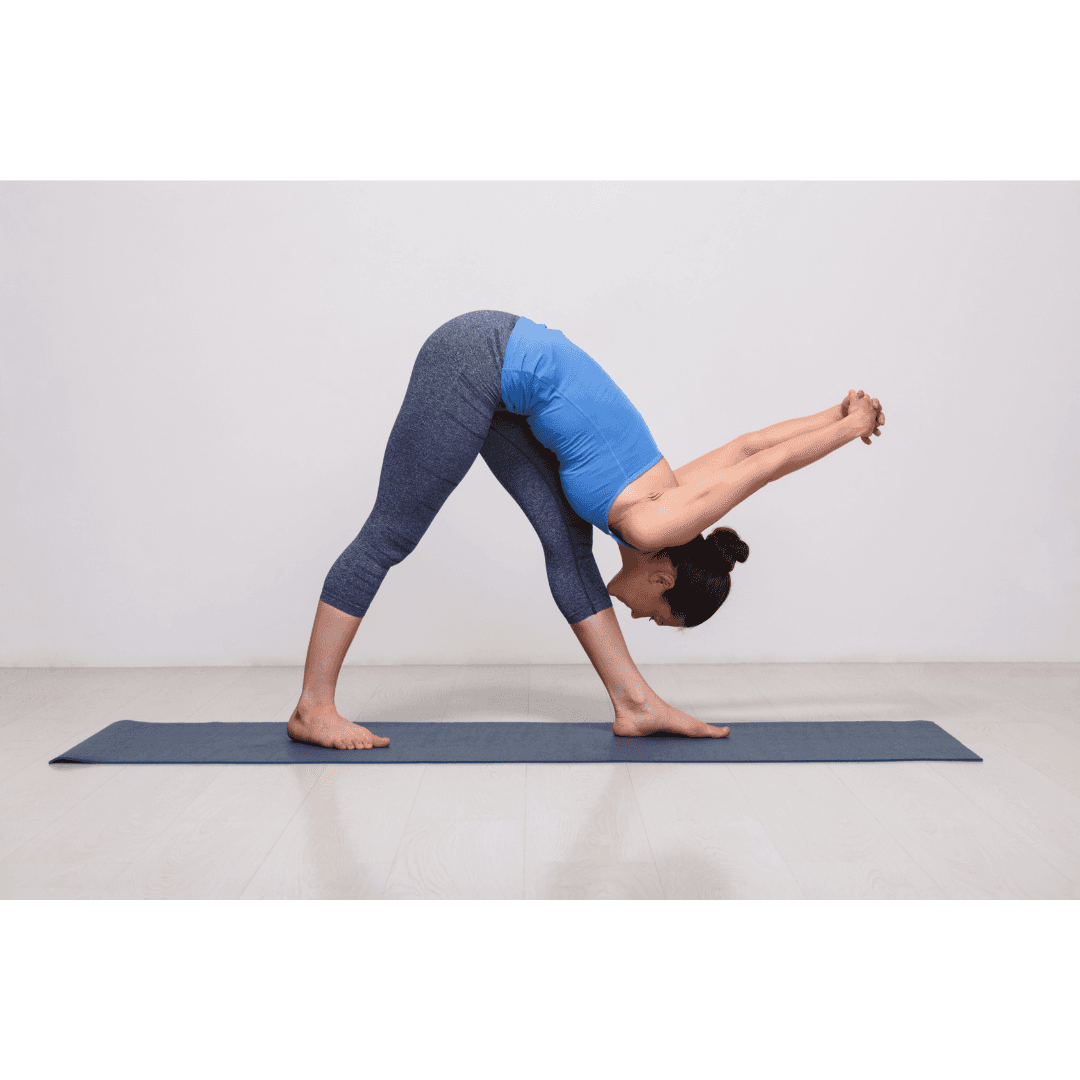
Both conditions feature generalized joint hypermobility—joints that bend and stretch far beyond the normal range. The key difference is that hEDS meets stricter diagnostic criteria, while HSD describes patients with significant hypermobility symptoms who fall just short of the full hEDS diagnosis.
Here's what many physicians don't realize: HSD and hEDS often require the same management approach. The label matters less than recognizing and treating the symptoms.
Why These Conditions Hide in Plain Sight
hEDS and HSD are masters of disguise:
No single telltale symptom exists. Symptoms overlap with dozens of other diagnoses, making pattern recognition difficult.
Symptoms fluctuate unpredictably. You might feel terrible one day and relatively normal the next.
Severity changes over time. Mild childhood "clumsiness" can evolve into debilitating symptoms during puberty or young adulthood.
This combination often leads to patients being dismissed as anxious, deconditioned, or told they're imagining their symptoms.
The Cost of Delayed Diagnosis
Professor Rodney Grahame, a leading expert on hypermobility disorders, estimates that approximately 95% of cases presenting to clinics are missed. When patients do get diagnosed, they've typically been searching for answers for 14 to 28 years.
The gender disparity is striking: women wait an average of 16 years for diagnosis, while men wait only 4 years—reflecting broader gender bias in healthcare.
What This Delay Costs
Those aren't just statistics. They represent:
Years of uncontrolled pain
Inappropriate psychiatric treatments for physiological problems
Preventable joint damage from misguided exercise recommendations
Psychological trauma from repeated dismissal and gaslighting by healthcare providers
Decreased quality of life when effective interventions exist
Current Diagnostic Criteria
It's outdated, but still used, but hopefully in 2026 we will get an update!
The 2017 International Consortium established criteria requiring three key elements:
1. Generalized Joint Hypermobility assessed through the Beighton scale—a simple, equipment-free test
2. Two of Three Additional Features:
Multiple signs of a broader connective tissue problem (from a specific list of 12 features)
At least one first-degree relative with hEDS
Chronic musculoskeletal issues like widespread pain or joint instability
3. Ruling Out Other Conditions, especially vascular EDS and other connective tissue disorders, such as rheumatology and autoimmune conditions - they can co-exist and confuse the symptoms!
Patients who have significant hypermobility and symptoms but don't meet all hEDS criteria receive an HSD diagnosis. Both deserve serious clinical attention and similar management strategies.
The Web of Related Conditions
hEDS and HSD rarely exist in isolation. Patients typically present with interconnected conditions that amplify each other:
#Musculoskeletal Issues
Chronic widespread pain, joints that partially dislocate (subluxations), TMJ dysfunction, and postural problems from poor proprioception—your body's sense of where it is in space.
#Autonomic Nervous System Dysfunction
Many patients develop POTS (postural orthostatic tachycardia syndrome), where heart rate spikes inappropriately when standing. This causes dizziness, presyncope, brain fog, and crushing fatigue. It's measurable and physiological—not anxiety.
#Gastrointestinal Complications
Slow gut motility, gastroparesis (delayed stomach emptying), severe bloating, and multiple food sensitivities—particularly to gluten and dairy.
#Immune System Overactivity & Histamine Issues
Mast cell disorders, such as Mast cell activation syndrome (MCAS) often present in patients with hypermobility. They can cause many symptoms, including allergy-like reactions, flushing, hives, and sometimes dangerous anaphylaxis to various triggers.
#Neurological Manifestations
Chronic migraines, small fiber neuropathy (burning or tingling sensations), and sometimes cervical spine instability with serious neurological symptoms.
#The Critical Point: These conditions interact. Dysautonomia worsens GI symptoms. Poor sleep exacerbates everything. MCAS triggers dysautonomia flares. Treating them in isolation often fails; addressing them together creates synergistic improvement.
Why Rheumatologists Are Key Players
Rheumatologists are uniquely positioned to recognize and coordinate care for hEDS and HSD:
We assess joint hypermobility routinely
We differentiate types of joint problems—inflammatory arthritis, autoimmune disease, or mechanical instability from hypermobility - there are many causes of joint pain and often can be present at the same time.
We think systemically about complex, multi-organ conditions and find solutions to treat them
We rule out conditions that mimic hEDS, like lupus and other autoimmune connective tissue diseases